Guest Writer
There is so much that happened in that first week when the family and I were trying to grasp what Dana was going through. When I re-read my notes, text messages, and talk about that first week, I am amazed that Dana lived through those first two nights. When I brought her to the ER in the early morning hours of July 17, I really thought she would be given an antibiotic and start to feel better in 24 hours. I had no idea of the nightmare that lay ahead.
July 17, 2018
8:09 a.m.
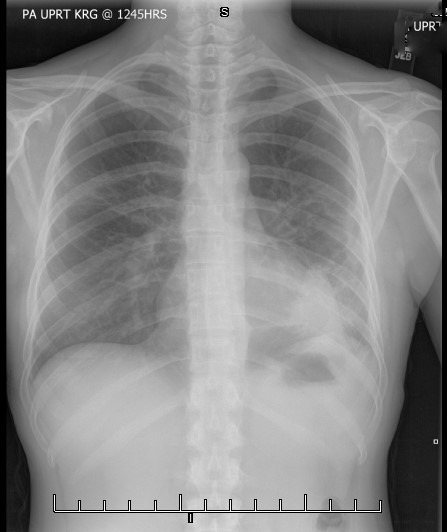
Me: Dana is in ICU with double pneumonia, blood infection. They just intubated her. She is sedated now. The family just got here but I’ve been here since 2:30 a.m.
1:49 p.m.
Me: They are keeping her sedated.
July 18, 2018
Me: She’s fighting for her life. I am going to the hospital this morning.
July 19, 2018
Me: 11:47 a.m. I won’t be in to work after all. They are seeing some improvements and trying a few new things so I want to be here. It is scary.
July 20, 2018
Me: 9:53 a.m. They have markers on her fingers and toes to see if the purple is decreasing or increasing. They are weaning her off more meds. She is still sedated.
NOTE: At one point there were 14 IV bags connected to Dana. Four of those bags were the vasopressors. We were told that normally a person has one or two vasporessors. Many on staff had never seen anyone with four pressors!
July 21, 2018
Me: 10:45 a.m. Doctor said Dana has hit rock bottom. She still has a breathing tube and she is not really coming out of the sedation.
July 22, 2018
Me: 8:47 a.m. Dana responded appropriately to commands for the first time in two days.
July 24, 2018
Me: 10:59 a.m. Bronchioscopy went well. A determination will be made this afternoon about whether or not the breathing tube can be removed.
5:02 p.m. The oxygen tube is out of her throat but she still has oxygen at her nose. She is very weak so her voice is barely a whisper. All her systems seem to be working. Her lungs are very congested with the pneumonia. She still is not getting food. She has an IV but it is not nutrition.
July 25, 2018
Me: 9:55 a.m. Doctor said Dana has to cough today and get rid of the mucus in her lungs or she will backslide.
9:11 p.m. Now the doctor says he might do a trachotomy tomorrow. Patients are not usually kept on a breathing tube longer than four days. Also, doctors usually skip a second intubation and go right for a tracheotomy. It makes it easier to return to eating regular food and being able to talk. It could be temporary or not.
July 26, 2018
Me: 9:19 a.m. The doctor just told Dana that she will need a tracheostomy. She is writing us notes now. She made a sad face but didn’t freak out. She probably didn’t grasp the situation.